Healthcare Costing in 2025: The Key to Financial Sustainability in a Shifting Reimbursement Landscape
by Ali Olleik
April 13, 2025
With strategic investments in costing infrastructure, Middle Eastern healthcare providers are well-positioned to thrive amid the challenges of 2025, creating a healthcare environment that prioritizes both fiscal responsibility and patient-centered care.
Why Costing Matters More Than Ever
In 2025, healthcare costing stands as a critical tool for healthcare organizations, enabling them to make informed financial decisions, optimize resources, and maintain financial sustainability amid rising costs. This approach becomes especially relevant as healthcare systems in the Middle East, especially Saudi Arabia and Oman, shift from traditional reimbursement models toward value-based care. Accurate and comprehensive healthcare costing not only provides insight into expenses and profitability but also supports quality care delivery by guiding budget allocation, pricing, and investment in medical technologies. The journey to sustainable healthcare begins with understanding the cost dynamics that shape patient services and operational processes.
The Financial Pressures on Healthcare Systems
The global healthcare landscape has seen substantial financial strain, and Middle Eastern healthcare systems are no exception. By 2025, healthcare costs in the region are expected to escalate due to an aging population, increased demand for chronic disease management, and the integration of advanced technologies. The UAE, for example, is projected to see healthcare spending increase by over 9% annually, driven by both population growth and lifestyle diseases, such as diabetes and cardiovascular conditions. With similar trends in Saudi Arabia, Kuwait and Oman, healthcare providers are pressed to operate efficiently without compromising patient care.
Accurate costing methodologies help healthcare organizations determine where resources are being expended most heavily, enabling cost-saving measures that target non-essential spending. Furthermore, as Saudi Vision 2030 and Oman Vision 2040 push for improved healthcare quality and accessibility, there is increased pressure to implement transparent, sustainable cost structures.
Shifting Reimbursement Models:
A Value-Based Revolution
Saudi Arabia and Oman are embracing value-based care (VBC) reimbursement models that reward healthcare providers for positive patient outcomes rather than the volume of services provided. This shift requires precise cost-tracking methods to link healthcare spending to outcomes, an area in which costing plays a pivotal role. The Saudi Health Council’s rollout of the Diagnosis Related Group (DRG) payment system is a prime example, rewarding providers based on the quality and efficiency of care delivered. This model necessitates a thorough understanding of patient-level costs to ensure that reimbursements align with actual expenses incurred.
Oman’s Ministry of Health has similarly introduced initiatives to transition toward outcome-based reimbursements, placing greater emphasis on preventive care and chronic disease management. The adoption of such models emphasizes the need for accurate healthcare costing systems that allow providers to align costs with the expected reimbursement rates for various services.
The Role of Costing in Supporting Strategic Decision-Making
Healthcare costing allows organizations to make data-driven decisions on resource allocation and operational efficiency. For instance, an effective costing system can help healthcare managers identify high-cost services that may not yield significant patient benefits, guiding them to optimize or even discontinue such services.
In Saudi Arabia, where health expenditure per capita is projected to exceed $1,000 by 2025, this strategic approach is indispensable. Costing insights can inform policy decisions around which services to subsidize or invest in, aligning with the country’s broader health goals under Vision 2030. Similarly, Oman’s healthcare system faces rising demands from an aging population and increased lifestyle diseases, where strategic costing plays a key role in ensuring that resources are invested in high-impact areas.
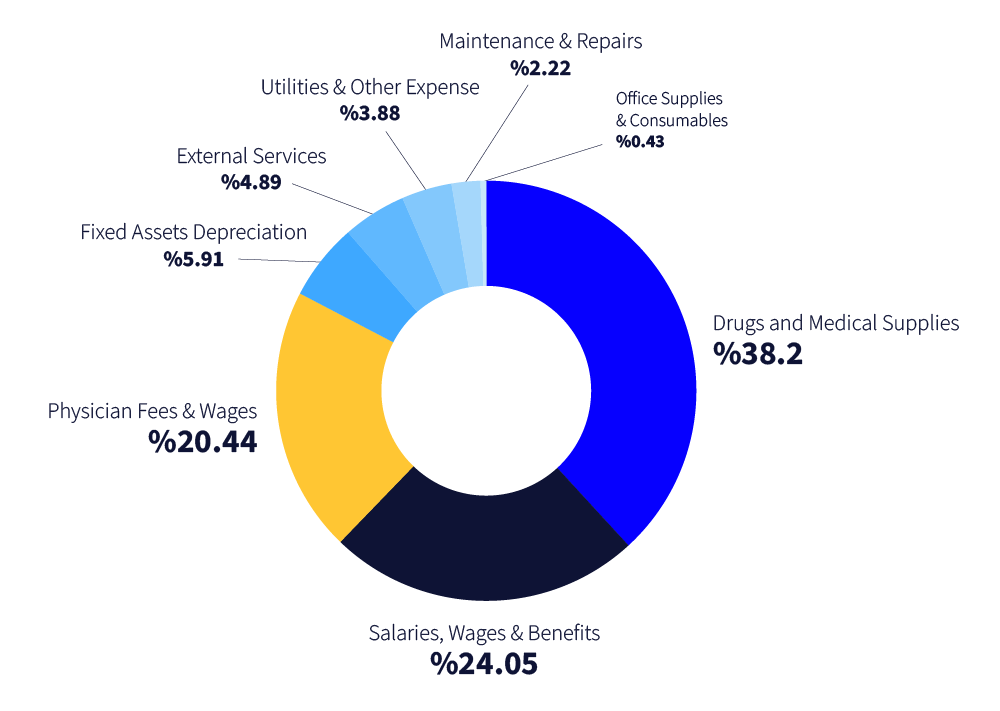
Almost 80% of hospital costs are incurred across 3 main cost categories.
Graph 01: Sample from a cost analysis study for a leading hospital in Kuwait
Source: GATES cost analysis team
How Data Analytics is Changing the Game
The role of data analytics in healthcare costing has gained momentum, allowing providers to monitor and manage costs with precision. In the Middle East, AI-driven analytics platforms are increasingly utilized to track service utilization, patient flow, and associated costs. For example, a recent study by HCA Healthcare in 2023 found that hospitals using data analytics tools reduced operating costs by up to 12% while improving patient outcomes, showing the value of a data-informed approach. By employing advanced technology, healthcare organizations can develop real-time costing insights that support transparent billing and optimize resource distribution.
The Road Ahead: Implementing Robust Costing Models for a Sustainable Future
The evolution of healthcare across the Middle East will depend on implementing robust costing models that respond to changing reimbursement requirements, population health needs, and financial pressures. Adopting Activity-Based Costing (ABC) or Time-Driven Activity-Based Costing (TDABC) can enable providers to gain a clear understanding of the true costs of care, fostering a financially sustainable healthcare model.
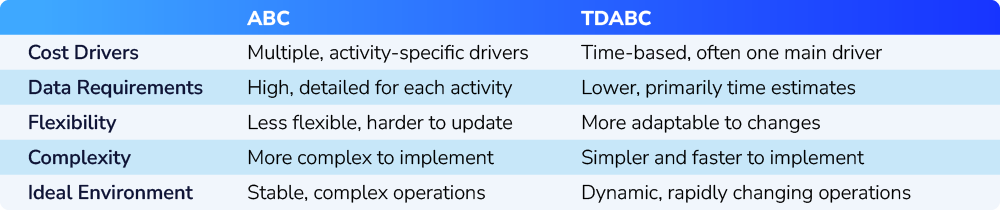
The two methods, ABC and TDABC, are both approaches to allocating costs based on activities rather than traditional cost allocation. However, they differ in complexity, data requirements, and approach to determining costs.
1) ABC:
Methodology: ABC assigns costs to products or services based on the specific activities involved in production or delivery. Each activity has an associated cost driver, such as machine hours or labor hours.
Complexity: ABC requires identifying and analyzing multiple activities and cost drivers, making it data-intensive and complex to implement.
Accuracy: It provides a detailed view of costs but can be less flexible in rapidly changing environments due to the static nature of its cost drivers.
Use Case: Best suited for organizations with a stable set of processes and a need for detailed activity-based insights.
2) TDABC:
Methodology: TDABC simplifies ABC by using time as the main cost driver. It estimates the time required for each activity and calculates cost based on the rate per unit of time.
Simplicity and Flexibility: TDABC is easier to implement as it doesn’t require detailed cost driver data. It adjusts more easily to changes, as the time required for activities can be quickly updated.
Accuracy: It is less detailed than ABC but more adaptable, allowing for faster recalculations with fewer data points.
Use Case: Useful for dynamic environments where process times vary, as it provides a more flexible and scalable costing approach.
Table 01: Key differences between ABC and TDABC methods
In summary, ABC provides a high level of detail but is more resource-intensive, while TDABC offers a streamlined approach that’s easier to update, making it suitable for businesses requiring quick adaptability. In Saudi Arabia, where the healthcare market is forecasted to reach $71 billion by 2026, these costing models can ensure that investments in medical technology, facilities, and personnel are strategically aligned with actual costs.
The Strategic Importance of Costing in Middle Eastern Healthcare
As the healthcare sector navigates through an era of reform and financial scrutiny, the importance of accurate costing has never been more pronounced. Costing enables healthcare providers in Saudi Arabia, Oman, and beyond to adapt to new reimbursement models, streamline operations, and improve patient outcomes while maintaining financial sustainability. As these countries continue to modernize their healthcare systems in line with national visions, the role of healthcare costing will remain essential in balancing the dual goals of economic efficiency and high-quality care. For Middle Eastern healthcare providers, the journey to sustainable, high-value healthcare starts with understanding—and optimizing—every cost.
About the Author(s):
Ali Oleik is the Strategic Partnerships Director of GATES Group in the Riyadh office.
Diyaa Faour is a Senior Cost Analyst in the Beirut office.